E. COLI O157:H7
SPECIMEN: Stool
REFERENCE RANGE: Negative
INTERPRETATION: Various E. coli strains can cause diarrhea. Enterotoxigenic E. coli (ETEC) produce enterotoxins and are a common cause of travelers diarrhea. Enteropathogenic E. coli (EPEC) do not produce enterotoxins or invade mucosa, but may cause prolonged diarrhea and are a cause of diarrhea outbreaks in nurseries. Enteroadherent E. coli (EAEC) cause watery diarrhea, particularly in travelers. Enteroinvasive E. coli (EIEC) cause high fever with bloody mucous stools and a toxic appearance. Enterohemorrhagic E. coli (EHEC), with its predominant serotype O157:H7, produce Shiga-like toxins which can cause bloody diarrhea and hemolytic-uremic syndrome.
E. coli O157:H7 causes a range of symptoms and clinical manifestations, as given in the next Table (Su C, Brandt LJ. Ann Intern Med 1995; 123:698-714):
Clinical Manifestations of E. Coli O157:H7 Infection
- Asymptomatic Carriage
- Nonbloody Diarrhea
- Hemorrhagic Colitis
- Hemolytic-Uremic Syndrome
- Thrombotic Thrombocytopenic Purpura
Incubation period is 1-8 days (typically 3-4 days). The illness begins with abdominal cramps and non-bloody diarrhea, and progresses over the next 1-2 days to bloody diarrhea. Most cases (95%) resolve over the next 5-7 days; 5% progress to hemolytic-uremic syndrome (HUS) (Mead PS, Griffin PM. Lancet 1998; 352:1207-12). The association of E. coli O157:H7 with clinical manifestations is given in the next Table (Su C, Brandt LJ. already cited):
Association of E. coli O157:H7 with Clinical Manifestations
| Clinical Condition | Percentage |
| All Cases of Diarrhea-Incidence | 0.6-2.4 |
| All Bloody Diarrhea or Hemorrhagic Colitis-Incidence | 15-36 |
| Development of Hemorrhagic Colitis with E. coli O157:H7 | 38-61 |
| Hemolytic Uremic Syndrome-Incidence | 46-58 |
| Progression to Hemolytic Uremic Syndrome | 2-7 |
Hemolytic Uremic Syndrome: Hemolytic uremic syndrome (HUS) is characterized by the classic triad of microangiopathic hemolytic anemia, thrombocytopenia, and renal failure. Various factors have been implicated in the development of this syndrome including genetics, pregnancy, drugs, toxins, chemicals, viruses, and bacteria. Primary transmission is via undercooked meat, but outbreaks have been associated with unpasteurized apple juice and fresh produce.
Typical cases present with a gastrointestinal prodrome of bloody or nonbloody diarrhea, often associated with abdominal cramps, vomiting, fever, and lethargy. Enterohemorrhagic E. coli, of which E. coli O157:H7 is the most prevalent serotype, is believed to account for more than 90% of all cases of HUS cases in industrialized countries (Siegler RL. Pediatr Clin North Am 1995; 42:1505-29). The natural history of post-diarrheal HUS is given in the next Table (Mead PS, Griffin PM. already cited):
Natural History of HUS
| Outcome | Percentage |
| Resolution | 60% |
| Proteinuria; Other Minor Sequelae | 30% |
| Chronic Renal Failure; Stroke; Other Major Sequelae | 5% |
| Death | 3-5% |
Testing: Specific testing for E. coli O157:H7 should be requested when this organism is suspected, but may be included on some standard laboratory stool culture evaluations. Unlike most other E. coli serotypes, O157:H7 forms colorless colonies on sorbitol-containing MacConkey agar because it does not ferment sorbitol rapidly. Suspect colonies are assayed for the O157 antigen using antiserum or latex agglutination testing.
Selected References: Mead PS, Griffin PM. “E. coli O157:H7″ Lancet 1998; 352:1207-12; Su C, Brandt LJ. “E. coli O157:H7 Infection in Humans” Ann Intern Med 1995; 123:698-714. Review of HUS: Siegler RL. “The Hemolytic Uremic Syndrome” Pediatr Clin North Am 1995; 42:1505-29.
Bakerman’s ABC’s Beta-Hydroxybutyrate
BETA-HYDROXYBUTYRATE
SPECIMEN: Red top tube, separate serum. Some methods use whole blood, serum, or plasma.
REFERENCE RANGE: 0.02-0.27mmol/L (0.2-2.8mg/dL). In diabetic ketoacidosis (DKA), ketoacidosis resolved <0.5mmol/L (<5.2mg/dL); ketoacidosis not resolved >1.1mmol/L (>11.4mg/dL) (Umpierrez GE et al. Diabetes Care 1995; 18:137-8). To convert international units in mmol/L to conventional units in mg/dL, multiply international units by 10.4.
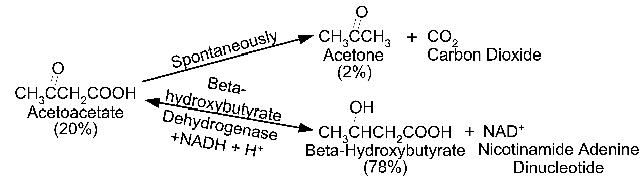
INTERPRETATION: The assay of beta-hydroxybutyrate is used as a measure of ketoacidosis. Beta-hydroxybutyrate is formed from acetoacetate as shown in the next Figure
Formation of Ketone Bodies
Ketones are formed in the conditions listed in the next Table:
Causes of Ketonemia
- C Diabetes Mellitus, Uncontrolled
- C Children: Acute Febrile Illness; Toxic States with Vomiting or Diarrhea
- C Alcoholism with Vomiting and Poor Food Intake
- C Ethanol or Salicylate Intoxication
- C Starvation, Prolonged
- C Some Weight Reducing Diets (High Fat, Low Carbohydrate)
- C Isopropyl Alcohol (rubbing alcohol)
- C Cortisol or Growth Hormone Deficiency
- C Secondary to Acidosis in Von Gierke’s Disease
- C Stress, Prolonged Exercise
Blood Ketone Testing: When ketone bodies accumulate, metabolic acidosis with anion gap develops. In diabetic ketoacidosis (DKA), fatty acid oxidation in the liver is stimulated by glucagon (in the absence of insulin). In addition, there is increased free fatty acid release from adipose tissues (see DIABETIC KETOACIDOSIS PANEL).
Specific assay for beta-hydroxybutyrate is the preferred method for diagnosing and monitoring treatment of ketoacidosis in diabetics (Amer Diabetes Assoc. Diabetes Care 2001; 24:S80-2). Ketoacidosis is considered to be cleared when beta-hydroxybutyrate level has fallen to <0.5mmol/L (Umpierrez GE et al. already cited).
Blood ketone measurement by the nitroprusside method (Ketostix, Acetest) measures only acetoacetate and acetone, and is not recommended by the American Diabetes Association. The nitroprusside method can underestimate the severity of ketosis when the ratio of beta-hydroxybutyrate to acetoacetate is high (eg, alcoholic ketoacidosis). This method may also indicate a lack of therapeutic response in DKA because the concentration of acetoacetate may increase while beta-hydroxybutyrate concentration decreases.
Some authors have questioned whether frequent monitoring with beta-hydroxybutyrate or other ketone assays add significant clinical information over routine measurement of serum glucose and total carbon dioxide in uncomplicated DKA (Porter WH et al. Am J Clin Pathol 1997; 107:353-8).
Urine Ketone Testing: Urine testing for beta-hydroxybutyrate is not available, and must be done by the nitroprusside method, which measures only acetoacetate and acetone(see further discussion in KETONE TESTING section).